1. Introduction
r. Balabhai Nanavati Hospital, blessed by Mahatma Gandhi, inaugurated by India's first Prime Minister, Jawaharlal Nehruin 1950 was reintroduced as Nanavati Super Specialty Hospital (NSSH).
Nanavati Super Specialty Hospital has been at the forefront of healthcare for the past 70 years.
As the COVID 19 pandemic struck our community, NSSH proactively took the initiative of systematically screening as well as triaging and getting ready to serve the community.
At NSSH, we made stringent protocols to segregate suspected cases, collect samples for testing and, if required, admit them in dedicated isolation units. The COVID-19 isolation wards & Isolation Intensive Care Unit was set up in a separate building to ensure the safety of other patients.
In the current dynamic scenario, the number of positive COVID-19 cases is on the rise, and guidelines need to be updated time and again. As a responsible medical facility, NSSH was gearing up to be prepared to provide continuous medical support in keeping with National and International standards. In its thirst for continual improvements, NSSH strived to serve the society at large and be in the frontline as CORONA WARRIORS.
We would like to discuss various steps taken by the administration in dealing with the COVID-19 crisis at a tertiary care hospital, along with the hurdles faced & the measures taken. We aim to share our experience & practice, which could be insightful to other hospitals, who would eventually have to face these challenges if an unprecedented surge does occur.
2. Few Facts
3. Role of Medical Administration
Considering the severity of the disease, Medical Administration geared up, and along with Chief Operating Officer, Executive Director, formed a multidisciplinary Task Force named Apex Committee. The committee prepared detailed process flows, conducted training sessions &initiated the process. Following were the objectives to start with: ? To devise standard Safety guidelines to be followed by all staff and to ensure that these guidelines were strictly adhered to by everyone with the help of regular training and audits. The final aim is to safeguard the health of the entire healthcare personnel and to prevent transmission to the vulnerable population.
? To form a Safety Team: comprising of representatives of Quality, Clinicians, Nursing staff, and Human resource department. The first step towards getting our hospital prepared was to establish an APEX committee for COVID care. The key members of this committee were:
Hospital Director and Chief Operating Officer: Their leadership and support ensured that all departments worked collectively.
The Director of medical services, Medical superintendent, Deputy Medical Superintendent and General manager, Operations: They organised and led the daily meetings and finalized decisions based on inputs from the multidisciplinary team. Their excellent leadership and decision-making were pivotal to the smooth functioning during the whole preparedness process.
Director of Critical Care, and Department Heads of Medicine, Emergency Medicine, and Surgery: These were the departments dealing with the patients directly. Coordination between various department heads, administrators, and their staff was essential for ensuring success of the planning process.
Chief Nursing Officer and Accreditation Coordinator, played a vital role in dealing with nursing issues for COVID patients, conducted regular training for staff for screening, Triage, and management of COVID patients.
Quality Manager and Hospital Laboratory and Infection Control Committee: who studied the ever changing guidelines from WHO, Ministry of health and family welfare, CDC, and implemented them effectively. Ensuring the safety of staff was very crucial to this plan. The most crucial and essential step to control the spread of the disease was to segregate COVID suspect patients from routine patients. We used case definitions and guidelines issued by the Ministry of health and family welfare (3).
4. COVID-19 Case Definitions (3) Suspect Case:
A patient with acute respiratory illness (fever and at least one sign/ symptom of respiratory disease (e.g., cough, shortness of breath) AND a history of travel to or residence of a country/area or territory reporting local transmission (See NCDC website for an updated list) of COVID-19 disease during the 14 days prior to symptom onset; OR A patient / Health care worker with any acute respiratory illness AND having been in contact with a confirmed COVID-19 case in the last 14 days prior to onset of symptoms; OR A patient with severe acute respiratory infection (fever and at least one sign/symptom of respiratory disease (e.g., cough, shortness of breath) AND requiring hospitalization AND with no other a etiology that fully explains the clinical presentation.
5. ORA case for whom testing for COVID-19 is inconclusive Laboratory Confirmed case:
A person with laboratory confirmation of COVID-19 infection, irrespective of clinical signs and symptoms.
Immediate measures were taken to isolate the patientas soon as a case was identified, and the concerned authorities were immediately notified.
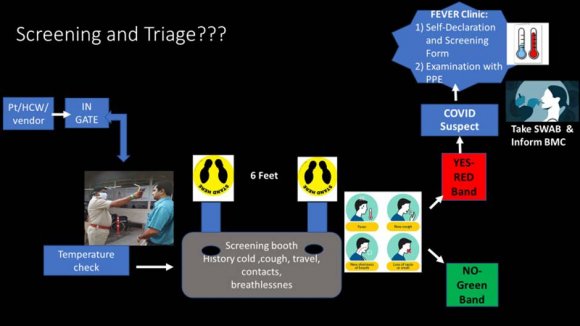
Screening Protocols were standardized, based on guidelines from respective authorities with timely amendments. Screening guidelines were updated with changes made accordingly in the screening checklist provided to all the personnel on screening duty.
Every Single Personnel entering the hospital (patient, visitor if any, healthcare staff, vendoretc.) was screened.
The temperature was checked immediately after entry; then personnel was sent to the screening booth for history using a screening checklist, to identify people with history of travel, contact or symptoms of acute respiratory illness(ARI) like fever, cold, cough, and breathlessness.
Multiple screening desks were available to ensure the fast transit of patients. The screening was done by trained healthcare personnel in recommended PPE (Personal Protective Equipment) Screening checklist (questions to ask and actions to take)-to rapidly identify and isolate suspect COVID-19 cases was provided to them along with extensive training.
Screening was done following social distancing guidelines. Patients were supposed to stand on stickers marked at least 6 feet apart.
Additional Doctors were stationed at the screening booth to further strengthen the process by identifying patients not disclosing all relevant history.
Anybody with a positive history was sent to the triage area (Fever/Flu clinic) where a detailed assessment was done to identify risk factors and severity of the disease. Patients were asked to fill a Self-Declaration form; wherein a checklist is available. Swabs were further collected for testingCOVID-19 as per the clinical condition &advice.
The patients were segregated into 1) COVID suspects -symptomatic stable or unstable (critical). 2) COVID Positive -symptomatic stable or unstable (critical). The symptomatic patients were admitted to COVID wards, and the critical patients with serious disease were admitted to COVID Intensive care units.
After the test results were available, patients were shifted to normal non-COVID wards if the test results were negative and screening HRCT Chest did not reveal COVID like findings. Isolation units with secluded beds had been created for COVID suspect and positive patients in a separate building.
6. Activities in Lockdown Period
On the evening of March 24th, the government declared a 21-day lockdown from midnight onwards to control the spread of COVID -19. (4)
The lockdown was further extended in phases, and India was under a nationwide lockdown till 31st May in the city. (5)The Ministry of Home Affairs released new guidelines called 'Unlock 1.0' that allow the opening of malls, restaurants, and religious places in all areas except the containment zones from June 8 th , 2020. (6)
The biggest challenge &in fact the need was to restrict the footfall to the Hospital, which could help social distancing & decrease the chances of infectivity.
All outpatient services were closed in an attempt to reduce footfall and prevent transmission. All elective procedures/investigations had been canceled/rescheduled. Only emergency cases were being managed like stroke, obstetric emergencies, myocardial infarction, neurosurgery cases, pediatric emergencies, etc. Patients on hemo dialysis and those requiring chemotherapy were offered care using proper precautions to ensure their safety as these patients are at risk due to immune suppressed status. Once patients were found to have risk factors, it was of utmost importance to segregate them from the routine patients and admit them in dedicated isolation wards. This required strategic planning and the management faced a dual responsibility here, to safeguard the health of already admitted patients and patients coming in for services like chemotherapy and hemo dialysis while making sure proper care was provided to the ones suffering from this dreadful disease. to ensure these, a separate building (Annex) within the hospital premises, which had an exclusive access, was designated as the isolation building. It had special COVID wards and Intensive care units.
7. Testing for COVID
8. Continue
The designated wards were made using guidelines which were followed strictly.
? The building had a separate entry and exit. ? Good ventilation; these areas were not a part of the central air-conditioning. ? A minimum distance of 1 meter maintained between adjacent beds in the designated Ward/ ICU. ? Lines of demarcation for restricted entry in the ward were put in place. ? The Donning and Doffing areas for PPE were separate. A shower facility was available.
? The Dirty Utility Area was segregated and dedicated to the Ward/ICU and not shared with any other area. ? Portable X-ray was placed inside the Ward and dedicated for the use of COVID 19 patients. ? The isolation wards/ICUs had a separate toilet with proper cleaning and supplies. ? Visitors were strictly not allowed in the isolation facility.
All healthcare workers working in these wards had to follow stringent safety protocols and exhaustive management guidelines. Doctors, Nurses, Housekeeping Staff, and administrators posted to isolation facility were dedicated and not allowed to work in other patient-care areas ? Healthcare workers in this ward are posted for 14 days with weekly offs and 6 hours duties. Swabs were sent between days 5 and 7 after the last working day. Doctors on duty were provided accommodation in a good facility nearby; expenses of which were borne by the management. encouragement to all the Consultants, Clinical Associates, Residents, and nursing staff. ? Teams were formed like a safety team to ensure proper use of PPES and safety protocols. General audits were held to assess the effectiveness of training sessions. ? The housekeeping staff was provided regular training and guidance as these are the ones who directly come in contact with biomedical waste. ? All healthcare workers were provided prophylaxis (hydroxychloroquine). NSSH was probably the first hospital to initiate this along with MAX Hospitals. ? Management protocols were designed for the treatment of COVID-19 patients, which were updated timely. ? All the patients were strictly monitored.
Routes for patient transfers: COVID-19 patients requiring investigations like CT scan or Magnetic Resonance Imaging (MRI) were transferred through a separate Brown corridor, which was created during every patient transfer. This required coordination from the entire staff, including administrative managers, doctors, housekeeping, cleaning team, etc. Safety precautions were taken, and sanitization was done immediately after the transfer of a suspected or positive patient.
Disinfection and Sanitization-strict protocols were laid down for cleaning and disinfection.
9. Training Training Training
Training was probably the most difficult and essential aspect of a successful preparedness plan. Detailed presentation with videos, graphics, etc made in English & Marathi for better understanding were made.
10. Training sessions
11. VI. Covid 19 -Staff Health & Safety Team
Caring for suspected/confirmed COVID 19 patients in the hospital posed a new set of challenges. Staff at the frontline needed to learn new skills, follow new patient care guidelines, deal with a never before encountered crisis, and, most importantly, protect themselves, their patients, and their co-workers from the spread of this highly virulent infection. No amount of infection prevention precautions was going to be enough; the minutest gap could lead to catastrophic consequences to staff and patients. The safety of healthcare workers, therefore, is of paramount importance. They are the organization's most valuable resource. NSSH is taking all efforts to ensure the best standardsofmedicalcareandstaffsafetyareputintoplacean dtoensurethehealthandwell-beingofthestaffas they navigate this challenging time. To check the effectiveness, learn about opportunities for improvements, and putim mediate corrective measures in placeona daily basis, we constituted "Staff Health and Staff Safety Team."
The team comprised of the following:
12. Process Flow of Imaging
Only emergency and semi emergency investigations were done .All elective procedures were canceled.
13. Following investigations were done:
? MRI-Indications like stroke, seizures, paediatric emergencies, etc. ? Ultrasound-obstetric scans, severe abdominal painureteric colic, appendicitis, obstruction, surgical indications like appendicitis, cholecystitis, and pediatric emergencies. ? CT scan-Stroke, trauma, severe breathlessness to rule out pulmonary thromboembolism
14. b) Prophylaxis
Prophylactic Hydroxychloroquine was given to all healthcare personnel, frontline as well as others Dose: Tablet Hydroxychloroquine 400 mg BD, followed by 400 mg once a week.
Management of accidental exposure in healthcare personnel-safety of the staff was our prime concern, but accidental exposures do occur, and their management had to be done swiftly. This included contact listing as well with the help of CCTV footage and questioning. Examination without adequate PPE.
? Anyone in proximity (within 3 ft.) of the confirmed case without precautions. Management of such High-risk contacts: Stop all health care interaction with patients for a period of 14 days after the last day of exposure. SWAB sent on day 5
15. Quarantine for 14 days d) Low risk-HCW wearing proper PPE(3)
Management: Self-monitor temperature and respiratory symptoms daily for 14 days after the last day of exposure to a COVID-19 patient and inform if symptoms occurred.
Reinforce contact and droplet precautions when caring for all patients. Guidelines provided by Mo HFW were utilized. (3) X.
16. Counseling and Psychological Support
Counseling staff was a major challenge as it was of utmost importance to maintain the morale of all healthcare staff working for COVID-19 patients. Patient counselling was another issue tackled by the aid of video/tele-services as patients in isolation were under mental and psychological stress away from families.
Counseling sessions were arranged for staff regularly.
17. Methods used:
? Tablets were provided to patients. Counseling was done using phone, Whats App, and video calls. ? Family Briefing and Counseling was arranged using electronic media like TAB video counselling. ? The consultant doctor in charge of the patient would engage with the family /attendant once a day and as and when required with documentation in family briefing form done onceevery day. The entire healthcare force has been under tremendous pressure during these times, not just physically but emotionally as well. Social distancing and quarantine measures have had an impact on psychology. Keeping the staff motivated throughout the whole process was very crucial. The management was trying to keep the morale high by arranging regular counseling sessions for all staff .Entertainment activities like singing sessions were organized for staff on weekends to lift their spirit. Video calls and other virtual methods of contact were advised between healthcare staff and supervisors for any guidance needed.
Change is inevitable but at the same time, adapting to change is difficult. Everything in our workplace has currently changed, but what keeps employees motivated and what employers and leaders can do remains the same, that is, to appreciate, encourage, and support. The administration strongly believed in this.
18. b) Digital health-Telemedicine
Digital health is turning out to be a promising solution currently. (8) Telemedicine has proved to be a key enabler during these difficult times.
Teleconsultation services were provided to patients with mild symptoms not related to COVID-19 and who did not need a hospital visit, using guidelines provided by the Ministry of health and family welfare and Maharashtra Medical Council (9, 10). During this pandemic, the utilization of tele health services certainly helped to slow transmission by reducing direct contact of patients with healthcare facilities, also enabling patients not suffering from COVID-19 to continue to receive care. This was particularly important for older adults, immune com promised patients and diabetics who were at the most risk during this pandemic.
For Radiology services, home workstations with remote access were provided to radiologists wherever feasible. Teleradiology made it possible for radiologists to view and report scans from their homes, thus protecting them from exposure while providing the Tele-technology also made it possible to conduct training sessions, administrative meetings, and educational activities effectively. Multiple webinars had been arranged by various academic groups throughout the country to ensure continuous learning was not hampered.
19. c) Challenges faced by the Medical Administration
COVID-19 pandemic brought with it many challenges having a deep impact on social life and the economy. NSSH took the initiative of screening and triaging all hospital visitors. The administration and management team of the hospital worked relentlessly to prepare an efficient strategy and make SOPS for proper management of hospital operations.
The economic impact faced by the hospital due to reduced footfall, closed OPDs, loss of international patients, and cancellation of elective procedures was going to be a tough one, but the primary aim was to safeguard the health and save lives. To ensure COVID preparedness, hospital expenditures also increased as funds had to be arranged for safety equipment like PPEs, cleaning and disinfection supplies, ambulances for patients. The fixed costs of running a hospital are immense. To manage these, while managing to pay staff salaries and ongoing operations were and are going to be tough tasks.
The number of positive COVID 19 cases are rising daily. The guidelines and strategies for testing, management, and screening provided by various authorities like ICMR, WHO, MOHFW, MCGM had to be thoroughly read and understood and appropriately updated time and again. As a responsible medical facility, NSSH was prepared to provide continuous medical support in keeping with National and International standards.
A nationwide lockdown was announced by the government to reduce spread of the disease. However, this also had an impact on healthcare facilities.
? Constant supply of Protective equipment's: PPEs, disinfection, and sanitization, arranging supplies for safety also was a concern as the stocks were not enough. This pandemic was an unprecedented one and preparation for this was not possible due to the already existing shortage of supplies in the market. Finding distributors and liasoning was a major concern. But we could overcome this with the support of Authorities. ? Staff movement and transportation -shut down of local transport caused difficulties to healthcare personnel to reach the hospital for duty. The hospital management arranged bus transportation for the staff& sought the help of Authorities for staff' transport.
20. Documentation
? The biggest challenge was to ensure documentation. In normal circumstances, the relatives were available for signatures after communication & counseling. In this COVID crisis, as the relatives were usually quarantined, it was very difficult for the doctors to maintain records .Various electronic media had to be used.
? Doctors in PPE faced a lot of practical difficulties to do the paperwork. Medical Administrative staff could do audits to check the documentation but in case of the COVID scenario , wherein papers could not be transferred to Non-COVID areas , it was difficult to do so. ? Psychological impact -Doctors, Staff Nurses, support staff administrators are human too! They have been called CORONA warriors, but this war has had a toll on all. Time away from families due to excessive work as also quarantine measures had surely affected all. The Management started communication on a daily basis and even were approachable in emergencies. There was constant dialogue, interaction with personnel & in some cases had one to one conversation with their families too.
Extensive research and study with long working hours away from family -strategy planning Prepare a COVID preparedness plan to manage COVID patients while ensuring safety and providing care for routine patients.
21. Challenges faced by the Medical administration
Deal with economic impact of the pandemic while maintaining staff morale and their financial security along with operations and preparedness expenditures Manage shortage of Supplies like PPE and liasoning with distributors/manufacturers Documentation In normal circumstances, the relatives were available for signatures after communication & counselling . In COVID crisis, as the relatives were usually quarantined , it was very difficult for the Doctors to maintain records . Electronic media had to be used . Practical difficulties faced by doctors in PPE while doing paperwork. Documentation audits by Medical Admin staff were difficult as papers could not be transferred to Non-COVID areas.
XI.
22. Conclusion
Tackling this pandemic has caused stress on hospitals everywhere, financial, psychological, and social. But there will be ways to weather this storm, and we must not lose hope. Doctors are the soldiers; the world will remember once this war is over. Our current priorities for COVID-19 preparedness should be to focus on early detection, limiting exposure, safety precautions, training, and maintenance of operations and staffing. Patience, calm minds, new administrative ideas and strategies, individual and cumulative discipline, a sense of solidarity, and a shared sense of purpose are all that we need currently to overcome these unprecedented and challenging circumstances.


















| ? To | strive | towards | Staff | motivation | and |
| encouragement. | |||||
| ? To develop Standardized, written protocols for |
| identifying, Segregating, Monitoring and, reporting |
| of COVID-19 patients. |
| ? All waste collected in different colored bags was |
| finally. |
| ? Placed in a double-layered yellow bag and sealed |
| after spraying 1%sodium hypochlorite over the inner |
| waste bags. |
| ? A dedicated collection bin labelled as COVID-19 |
| was used to store COVID-19 waste and keep |
| separately in temporary storage room before |
| handing over to authorized staff. |
| ? Separate record of waste generated from COVID-19 |
| isolation wards was main tained. |
| ? The surface of containers/bins/trolleys used for |
| storage of COVID-19 waste were disinfected with |
| 1% sodium hypochlorite solution daily. |
| VII. |
| Acknowledge tough situations and recognize |
| accomplishments, even small ones. |
| ? Provide help with basic needs, such as |
| transportation. |
| ? Monitor each other's workload and encourage each |
| other to take breaks. |
| ? Communicate your buddy's requirements and their |
| limitations to the managers -try to make your |
| buddy feel "safe" to speak up. |
| ? The Staff Health & Safety Team conducted daily |
| audits, immediately started doing closures of the |
| Audit findings ; training was continued . |
| a) Infectious waste management |
| Biomedical waste management is probably the |
| most challenging aspect of this entire process. Waste |
| management was done following guidelines as per |
| BMWM rules, 2016, Ministry of Health and Family |
| Welfare guidelines (Mo HFW) |
| 28 Global Journal of Management and Business Research Volume XX Issue XI Version I Year 2020 ( ) A | Precautions Screening history Full PPE Cleaning and disinfection with settling time in between cases at least 20 min Informed consent to risk of COVID 19 High risk consent for procedures OT staff to wear Full PPE The Discharge Policy for Covid Cardiac patients with symptoms Trauma Vascular indications Obstetric emergencies Stroke Cancer /Dialysis Surgical emergencies-appendicitis/cholecystitis Positive Patients ? Criteria and guidelines have also been laid down for IX. discharge of positive patients. We follow MCGM guidelines for the discharge. Care was being taken that they were asymptomatic, No worsening of CXR. ? SPO2 > 95% on RA ? Respiratory/Flu clinic/Screening Area Dedicated COVID Hospital S. No. Setting Activity Risk level PPE 1 Screening at entrance of hospital Triaging patients, history, provide triple layer mask to patients, Screen patients, offer hand sanitization, check temperature Moderate ? N 95 mask ? Gloves ? Surgicalgowns 2 Front Office/Reception /Security Provide information to patients Registration Billings Moderate ? N 95mask ? Gloves 3 At Triage / Respiratory / Flu Clinic Nursing Counter Record temperature with handheld thermal recorder, Screening history Moderate ? N 95 mask or FFP 2 equivalent ? Isolation Gown (Full Head to Toe) ? Gloves ? Eye Protection (goggles/visor) 4 Doctor Chamber in Triage / Respiratory /Flu Clinic Clinical Management (Doctors, Nurses) Moderate ? N 95 mask or FFP 2 equivalent ? Isolation Gown (Full Head to Toe) ? Gloves ? Eye Protection (goggles/visor) Sample Collection Room in Triage / Resp / Flu Clinic Taking sample COVID 19 High ? N 95 mask or FFP 2 equivalent ? Isolation Gown (Full Head to Toe) ? Gloves Anesthesia ? Eye Protection (goggles/visor) ? Eye Protection (goggles/visor) Housekeeping Staff in Triage / Resp / Flu Clinicarea Cleaning frequently touched surfaces/ Floor/ Cleaning Linen Moderate ? N 95 mask or FFP 2 equivalent ? Isolation Gown (Full Head to Toe) ? Heavy duty gloves ? Eye Protection (goggles/visor) OPD Dedicated COVID Hospital Setting Activity Risk level PPE 1 Front Office/Reception /Security Provide information to patients Registration Billings Moderate ? N 95 mask Gloves 2 Chamber of Dental/ENT doctors/ Ophthalmic doctors Clinical management Moderate ? N 95 mask or FFP 2equivalent ? Isolation Gown (Full Head to Toe) ? Gloves 1 Green Emergency Unit Attending Emergency cases ? Moderate ? N 95 mask or FFP 2 equivalent ? Isolation Gown (Full Head toToe) ? Gloves ? Eye Protection (goggles/visor) Green / Red Emergency Unit Attending Emergency cases when Aerosol Generating Procedures are anticipated ? High ? Full complement of PPE ? N 95 mask or FFP 2 equivalent ? Isolation Gown (Full Head to Toe) ? Gloves ? Eye Protection (goggles/visor) 3 Red Emergency Unit Isolation (For suspect or confirmed COVID cases) Attending to severely ill patients of suspected or confirmed COVID 19 High ? Full complement of PPE ? N 95 mask or FFP 2 equivalent ? Isolation Gown (Full Head to Toe) ? Gloves ? Eye Protection (goggles/visor) Day Care Facilities Dedicated COVID Hospital ? Eye Protection (goggles/visor) 4 Operation Theatre And Cath lab Performing Surgery, procedures administering ? Gloves High ? N 95 mask or FFP 2equivalent ? Isolation Gown (Full Head to Toe) OTHER Services Dedicated COVID Hospital S. No. Setting Activity Risk level PPE 1 Housekeeping Staff Cleaning frequently touched surfaces/ floor/ changing Linen Moderate ? N 95 mask or FFP 2 equivalent ? Isolation Gown (Full Head to Toe) ? Heavy dutygloves ? Eye Protection (goggles/visor) 2 CSSD /Laundry Cleaning, disinfection, sterilization Moderate ? N 95 mask or FFP 2 equivalent ? Isolation Gown (Full Head to Toe) ? Heavy dutygloves ? Eye Protection (goggles/visor) Administrative, Financial COVID Challenges: 5 ? Eye Protection (goggles/visor) 3 Pre-anesthetic check-up clinic Clinical examination Moderate ? N 95 mask or FFP 2equivalent ? Isolation Gown (Full Head to Toe) ? Gloves ? Eye Protection (goggles/visor) 4 Antenatal Clinic Clinical examination Moderate ? N 95 mask or FFP 2equivalent ? Isolation Gown (Full Head to Toe) ? Gloves ? Eye Protection (goggles/visor) 5 All other OPDs Clinical examination Moderate ? ? Isolation Gown (Full Head to Toe) ? ? Eye Protection (goggles/visor) 6 Pharmacy counter Drugs issue and billing Mild ? Triple layer medical mask ? Gloves 7 Sample Collection Room for non COVID Sampling Samples for lab testing NA ? NA 8 Visitor's accompany ng young Children and Elderlies Support in navigating various service areas Mild ? Triple layer medical mask Emergency Dept. Dedicated COVID Hospital S. No. Setting Activity Risk level PPE IPD Services Dedicated COVID Hospital S. No. Setting Activity Risk level PPE 1 Isolation Ward: Individual Isolation rooms/ cohorted isolation rooms/ ward Clinical Mgmt. High ? N 95 mask or FFP 2equivalent ? Isolation Gown (Full Head to Toe) ? Gloves ? Eye Protection (goggles/visor) 2 ICU Critical care High ? Full complement of PPE ? N 95 mask or FFP 2equivalent ? Isolation Gown (Full Head to Toe) ? Gloves ? Eye Protection (goggles/visor) 3 Labor room Intra-partum care High ? N 95 mask or FFP 2equivalent ? Isolation Gown (Full Head to Toe) ? Gloves services ? Eye Protection (goggles/visor) Gloves 3 Radiotherapy & Other Day care ? Gloves High ? Isolation Gown (Full Head to Toe) N 95 mask or FFP 2equivalent 2 Dialysis Dialysis High ? N 95 mask or FFP 2 equivalent ? Isolation Gown (Full Head to Toe) ? Gloves ? Eye Protection (goggles/visor) Chemotherapy& ? N 95 mask or FFP 2 equivalent S. No. Setting Activity Risk level Engineering, Security, Vendors, PPE 1 Bronchos copy and Endoscopy Aerosol generating ? Eye Protection (goggles/visor) Procedures High ? ? ? Gloves etc. Isolation Gown (Full Head to Toe) outdoor staff (valets, drivers) N 95 mask or FFP 2 equivalent 3 Other supportive Services Students, Volunteers, Candidates for interviews, Staff at Food outlets Mild ? Triple layermask | 29 Year 2020 Global Journal of Management and Business Research ( ) A Volume XX Issue XI Version I | |
| © 2020 Global Journals | © 2020 Global Journals | ||